ESAIC News
EA20 Newsletter: Abstract 4823: sustaining life to facilitate organ donation – in whose best interest is this, in the new UK opt out donor system?
Submitted abstract
In an abstract presented at this year’s Euroanaesthesia, doctors question in whose best interest is a life-sustaining treatment to facilitate organ donation, in light of the UK’s new ‘opt out’ system that presumes that all people are potential organ donors unless they have opted out.
“Our case highlights the ethics underlying life-sustaining treatments to facilitate organ donation, and where a line should be drawn such that interventions delivered still constitute the patient’s best interests,” say the authors, who include Dr Nia Evans, Junior Doctor at Cwm Taf Morgannwg University Health Board, UK, Dr Atul Garg and Dr. Viktorija Cerniauskiene, Intensive Care Consultants at Walsall Healthcare NHS Trust, Walsall, UK.
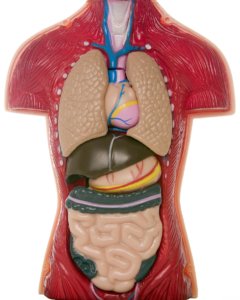
Organ donations come from the death of donors in two different ways: Organ Donation after Brain Death (DBD) and Organ Donation after Circulatory Death (DCD). In DBD, the person has no measurable brain activity, and has been declared brain dead, and is kept on life support while their organs are removed. In DCD, the person’s heart has stopped, and they have no pulse or other signs of circulation. Five minutes after this, death can be declared, and the person’s organs are removed across the following one to two hours.
However, worldwide, DBD is declining because the conditions that lead to brain death are limited. In most cases, brain bleeding (for example intracerebral haemorrhage – a type of stoke) or traumatic brain injury lead to brain death. Because of better prevention (progress in road safety legislation, safer cars, advances in arterial hypertension disease treatment) and treatment options, DBD numbers are declining.
In this case study, the authors discuss their patient, who was a 56-year-old male, who had a cardiac arrest in October of 2019, resulting in an irreversible brain injury from which he would never recover. In intensive care, he had a “Do Not Attempt Cardiopulmonary Resuscitation” order in place and a plan for DCD. Following a sudden deterioration into ventricular tachycardia (a very fast heart rate), drugs including amiodarone and vasopressors were given to stabilise him and provide more time to ensure organ viability for DCD.
Despite these life-prolonging treatments, the period of instability he had suffered deemed him unsuitable for donation. Put more simply, the patient’s blood pressure couldn’t be maintained at the desired level to ensure that his organs received enough blood and oxygen. This can make organs not suitable for donation, meaning they wouldn’t work if transplanted.
The authors explain that preparation for donation through DCD, as happened in this case, may take at least a few hours (approaching the family to confirm it is fine to proceed, multiple blood tests, and the organ retrieval team has to arrive at the donating hospital and set up theatres). “If a patient dies because of any reason, for example, tachycardia, while preparations are taking time, the donation can’t happen,” they explain.
“Our patient was becoming increasingly unstable, requiring drugs to control the high heart rate and high doses of inotropes to sustain life by keeping his heart beating. We are raising the question: is it is ethical to enhance and prolong life-sustaining treatment with an aim to facilitate organ donation, while these preparations are taking place if the patient has not specifically said they want to be an organ donor?”
They add: “In this case, it was decided to initiate amiodarone and vasopressors as a life-sustaining treatment for the sole purpose of organ donation.”
The authors point to UK Legal Guidance stating the maintenance of life-sustaining treatments is ethical if there is no harm or distress caused to the patient or family. However, the Consensus Statement on DCD from the British Transplant Society and Intensive Care Society consider the appropriateness of initiating new treatments such as inotropes to be unclear. They say: “As our patient was on the organ donor register it could be argued that treatment decisions were ethical, as they were in his best interest.”
“However, now the UK has transitioned to an ‘Opt-Out’ policy for organ donation in 2020 to tackle deficits ineligible donors. This will add further ambiguity to the ethical dilemma because it will no longer be appropriate to presume that the patient has consciously chosen to be on the organ donation register. Therefore, life-sustaining treatments such as those given to our patient may not now be in their best interest.”
They conclude: “Although life-sustaining treatment for the sole purpose of organ donation can increase the organ donor pool, it is highly contentious. Existing guidelines do not provide a clear framework to guide clinical decision-making. Therefore, decisions should be made on a case-by-case basis. The UK’s 2020 ‘Opt-Out’ policy likely is likely to make such decisions even more complex.”
Professor Julian Savulescu, Director of the Oxford Uehiro Centre for Practical Ethics at the University of Oxford, UK (who is not connected to this research) adds in a comment: “We need to get beyond this outdated idea that medical treatment should only be provided in the patient’s best interests. Sometimes it is provided out of respect for their autonomy, sometimes for the benefit of others. Keeping brain-dead patients’ organs functioning is not in their interests – they are dead. What matters is – are they suffering? If not, doctors can sustain their organs for the benefit of others. The new opt-out system doesn’t change that. People who are dead, or imminently dead, have no further use for their organs. But they are literally life-saving to large numbers of other people.”
Notes
This article is based on poster presentation 4823 at the Euroanaesthesia congress held online this year. The research has not yet been submitted to a medical journal for publication.
For full abstract, click here
For full poster, click here
For video presentation that accompanies the poster, click here
For more on DCD as it relates to this article, see the UK NHS Blood and Transplant guidance: Donation after Circulatory Death. https://www.odt.nhs.uk/deceaseddonation/best-practice-guidance/donation-after-circulatory-death/.
Read More of our special newsletter covering our virtual congress
Visit our COVID-19 Resource Hub for other news and resources.