Newsletter 2022
Newsletter April 2022: The Utility of Smart-Devices in Diabetic Patients during the Perioperative Period
Byron Rosero-Britton, Sebastian Amaya, Gabrielle Amaya, María José Andrade
sebass13@live.com
Technological advancements in the 21st century have allowed for a significant evolution in medicine. However, certain devices may be overlooked in specific settings, as is the case for smart devices in diabetic surgical patients. Smart devices have proven to have promising potential within medicine, as they are devices that are becoming very accessible, allow real-time continuous monitoring of physical activity and physiological monitoring, and allow for personalised reminders, among other functions1.
In 2022, an estimated 67 million individuals in the United States will be using some kind of wearable device, with smartwatches accounting for > 50% of devices2. Rawassizadeh et al. predicted the growth of smartwatch demand to 214 million units in the year 20183, with currently 13% of people in the United States having smartwatches, and 40% expressing their interest in purchasing one4. Users with smartwatches can access data such as steps, flights of stairs climbed, distance walked, hours standing, estimated energy expenditure, blood oxygen saturation and heart rate, all of which are readily available for interpretation5. Additionally, these devices can even inspire users’ motivation, engagement and interest in physical activity, thus creating habits leading to an increase in physical activity and decreased sedentary behaviour6.
Likewise, many interactive health applications for smartphones exist, such as blood glucose monitoring, via wireless connection with continuous glucose monitoring devices (CGM). Some of the most common current models that are compatible with CGM devices include the Apple Watch, Android Wear, Fitbit (Pebble), and Samsung7. Various current studies exist supporting longitudinal monitoring of health and analysis of wellness trends using smartwatches, as well as monitoring lifestyle habits such as time spent lying in bed versus walking around, by using the various technological parameters within the smartwatch programming such as daily step count8,9,10.
Currently, patients diagnosed with diabetes must monitor their blood-sugar levels via pin-prick blood tests or invasive under-the-skin CGM, which are currently good solutions, however, they have certain limitations such as cost-effectiveness11. Current literature has even shown that displaying the exact glucose values to users can improve logical reasoning and influence eating habits and activity, as well as impact favourably on glycaemic control12,13. With this in mind, we ask: what use could smart devices bring to the perioperative setting in diabetic surgical patients?
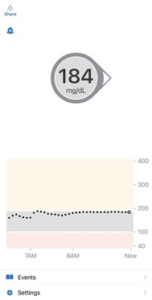
Figure 1. Glycaemic Monitoring Application on Smartphones on an Hourly Basis. Interphase of the Dexcom 6 glycaemic monitoring application for iPhone on an hour-to-hour basis
Beginning with the preoperative setting, smart devices can possibly help better gauge a patient’s physical status, and be used in unison with current questionnaires and other laboratory results, allowing us to interpret statistics such as blood oxygen saturation, glycaemic control (Figures 1 & 2), distance walked on average, and heart rate, among other factors, leading to a more objective analysis over a longer period of time. These devices allow us to take a live look at the patient’s actual physical status, rather than a subjective momentary questionnaire that may be dependent on the patient’s recall capacity. For example, we can draw fasting blood glucose to evaluate the patient’s current glycaemic control versus viewing the haemoglobin A1C or various glycaemic levels over a period of time, which will give us a view of the patient’s glycaemic control over the past few weeks or months, and a better understanding of their current metabolic control.

Figure 2. Glycaemic monitoring application on Smartphones throughout 24 Hours. Interphase of the Dexcom 6 glycaemic monitoring application for iPhone on a 24-hour basis
These situations can boost our argument that smart devices can assist us in giving us a more objective, and long term view of a patient’s physical wellbeing during the preoperative consultation.
Focusing now on the postoperative period, smartwatches can assist with alerts, reminding patients to walk several times throughout the day (allowing for prevention of deep vein thrombosis), breathing exercises (atelectasis prevention) and various other activities that can aid inadequate postoperative recovery and assist in meeting the various enhanced recovery after surgery (ERAS) goals. As mentioned previously, many smart devices have begun to integrate CGM-linked apps, allowing users to quickly and constantly check their blood glucose levels. This same technology can possibly be integrated into monitors, allowing the healthcare staff to constantly be updated on the patient’s glycaemic control without the need for constant pin-pricks, whether it be in the post-anaesthesia care unit or intensive care unit.
Additionally, it is important to highlight the use and relevance of these tools mentioned in paediatric diabetic patients since the diagnosis of patients with metabolic syndrome (including type 2 diabetes mellitus and obesity) are increasing14. This population tends to have less adherence to established treatments, so the use of smartwatches should be included in the postoperative scenario in order to improve blood glucose levels and also avoid multiple pin-pricks that can complicate blood glucose measurement.
Likewise, the newer generations are much more inclined towards the use of these technologies and tend to improve both preoperative and postoperative follow-up glycaemic control15. Finally, as general recommendations in the perioperative management of diabetic patients who undergo both elective and emergency surgery, certain pillars must be taken into account that provides an adequate balance and general well-being to guarantee an adequate recovery and correct wound-healing16. These recommendations include blood glucose control since increased values favour infections and inadequate healing in diabetic patients17.
We believe that smartwatches and similar devices can possibly be useful instruments, which deserve consideration for their use to better objectify certain criteria in the preoperative setting, as well as create better patient adherence to postoperative protocols, thus leading to a higher quality patient care. Therefore, we would like to encourage our international colleagues to partake in further studies with these devices in order to better understand the role of smart devices in the perioperative setting in the context of glycaemic control in diabetic patients.
References
- Reeder B, David A. Health at hand: J Biomed Inform. 2016;63:269-276. doi:10.1016/j.jbi.2016.09.001
- Koch L. – https://www.emarketer.com/content/the-wearables-series-millennials-infographic. Published 2021. Accessed August 5, 2021.
- Rawassizadeh R, Price BA, Petre M. 2014. Commun. ACM 2014; 58 :45–47.
- Lamkin P. https://www.forbes.com/sites/paullamkin/2018/02/22/smartwatch-popularity-booms-with-fitness-trackers-on-the-slide/?sh=a97a1937d96d. Published 2021. Accessed August 5, 2021.
- Massoomi MR, Handberg EM.. Eur Cardiol. 2019;14:181. Published 2019 Dec 18. doi:10.15420/ecr.2019.02
- Yen HY, Huang HY.. Perspect Public Health. 2021;141:89. doi:10.1177/1757913921989389
- Chesak, J. Diabetes Mine Team. 2020. Accessed 17 November, https://www.healthline.com/diabetesmine/wrist-smartwatches-and-diabetes-tech
- Jovanov E. Annu Int Conf IEEE Eng Med Biol Soc. 2015;2015:865. doi:10.1109/EMBC.2015.7318499
- Auepanwiriyakul C, Waibel S, Songa J, et al.. Sensors (Basel). 2020;20:7313. Published 2020 Dec 19. doi:10.3390/s20247313
- Sardana M, Lin H, Zhang Y, et al. J Med Internet Res. 2021;23:6,e25591. Published 2021 Jun 24. doi:10.2196/25591
- Grimes, K. Babylon. 2020. Accessed 17 November, https://www.babylonhealth.com/blog/tech/how-smart-watches-and-ai-can-help-people-with-diabetes
- Peters, E., Slovic, P., Västfjäll, D et al.. Judgment and Decision Making, 2008; 3: 31.
- Osborn CY, van Ginkel JR, Marrero DG, et al. JMIR Mhealth Uhealth. 2017;5:e179. Published 2017 Nov 29. doi:10.2196/mhealth.8781
- Hoogwerf BJ. Med Clin North Am. 2001;85:1213. doi:10.1016/s0025-7125(05)70373-4
- Del Castillo, Ana Sofía, Holder, Troyet al. (2011). Colombian Journal of Anesthesiology, 2011;39:56. https://doi.org/10.5554/rca.v39i1.76
- Simha, V., & Shah, P.. JAMA 2019; 321: 399.
- Fitzgerald, R, DPM, AACFAS. Global learning network. 2011. Accessed 17 November, https://www.hmpgloballearningnetwork.com/site/podiatry/how-address-post-op-infections-patients-diabetes
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter” ]











